Today I want to talk about a crucial topic that is often underestimated: the influence of hormones on bone, joint and muscle pain.
As a trauma specialist in musculoskeletal injuries and pathologies here in Tijuana, I see patients daily in my office seeking relief for these problems. It's essential to understand how hormonal imbalance can be an underlying factor in the chronic pain they experience.
Endocrine System
The endocrine system is composed of a network of glands that create and release hormones, including the pituitary gland, adrenal glands, thyroid, pancreas and ovaries among others.
Hormonal Imbalance and Metabolic Disorders
When the body produces too little or too much hormone or has problems receiving or processing them, a domino effect occurs. A hormonal imbalance can trigger a metabolic disorder, altering the body's normal functioning.
Some conditions related to hormonal imbalance and metabolic disorders include:
Diabetes
Metabolic syndrome
Tumors
Thyroid cancer
Hyperthyroidism and hypothyroidism
Thyroid nodules
Amenorrhea (absence of periods)
Hormonal acne
Infertility
Hypogonadism
Menopause disorders
Polycystic ovary syndrome
Premenstrual syndrome
Hypercalcemia and hypocalcemia
Osteopenia and osteoporosis
Vitamin D deficiency
Which hormones are related to bones?
Here are the crucial hormones for your bone health:
1,25-dihydroxyvitamin D: Calcium-regulating hormone, produced from vitamin D, necessary for calcium absorption.
Calcitonin: Protects against excessive calcium levels in the blood.
Sex hormones: Estrogen is a key regulator of bone remodeling in women and men, acting on cells that form and resorb. Testosterone is important for bone growth and is also a source of estrogen in the body.
Growth hormones: Growth hormone and its production of insulin-like growth factor (IGF-1) influence bone formation.
Thyroid hormones: Necessary for skeletal maturation and influence the maintenance of adult bones.
Cortisol: Large amounts of this adrenal hormone block bone growth.
Insulin: Important for bone growth, regulates both bone formation and resorption.
Leptin: This circulating hormone has direct and indirect influences on bone metabolism.

How endocrine diseases cause pain in bones, joints and muscles
Imbalances in calcium and phosphorus metabolism:
Hyperparathyroidism: Excess parathyroid hormone (PTH) raises calcium levels in the blood by extracting it from bones. This weakens bones (osteopenia, osteoporosis) and can cause diffuse bone pain, fractures and kidney stones. Joint pain is also common.
Hypoparathyroidism: PTH deficiency causes low calcium and high phosphorus levels in the blood. This can lead to painful muscle spasms (tetany) and, long-term, calcium deposits in soft tissues, including joints, causing pain.
Vitamin D deficiency: Vitamin D is essential for calcium absorption. Its deficiency (osteomalacia in adults and rickets in children) causes soft, weak bones, resulting in generalized bone pain, muscle weakness and deformities.
Thyroid hormone alterations:
Hypothyroidism (underactive thyroid): Low thyroid hormone production can lead to several musculoskeletal problems:
- Hypothyroid myopathy: Weakness, stiffness, cramps and diffuse muscle pain.
- Joint pain: Stiffness and pain in joints, especially hands and knees, often with swelling.
- Carpal tunnel syndrome: Nerve compression in the wrist, causing pain, numbness and tingling in the hand.
Hyperthyroidism (overactive thyroid): Excess thyroid hormones can also affect muscles and bones:
- Osteoporosis: Accelerates bone remodeling, which can lead to bone density loss and increased fracture risk.
- Muscle weakness: Weakness in proximal muscles (shoulders and hips).
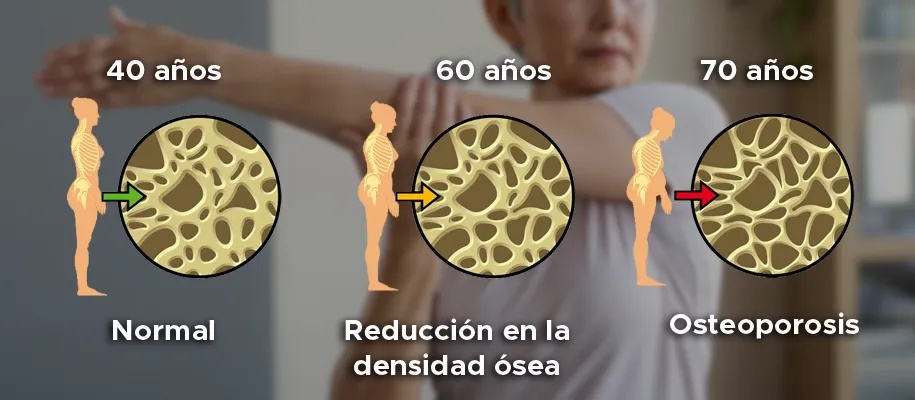
Osteoporosis due to hormonal imbalance
Osteoporosis is responsible for a large number of fractures, especially of the hip, spine and wrists, which frequently cause severe disability.
This condition usually occurs in postmenopausal women, although it can also affect patients with estrogen deficiency and those receiving corticosteroid treatment.
A 2017 Australian study on the "Prevalence of osteoporosis and age-related fragility fractures" revealed that osteoporosis risks in women increase progressively: from 45-49 years there is a 3.3% risk, increasing to 50% around 85 years.
Accelerated bone loss after menopause: Type 1 primary osteoporosis
In the first 5 to 7 years after menopause, reduced estrogen causes faster bone mass loss.
Why does this happen?
An imbalance is created between bone resorption and production at both estrogen and estradiol levels, which drops by 10-15% and estrone by 35%. This causes the calcium that is normally well "stored" in bones to begin releasing into the blood. To prevent too much calcium accumulation, the body increases its elimination through urine, absorbs less calcium from food and adjusts the production of certain hormones related to its management.
Afterwards, the rate of loss slows down, entering a phase known as type II osteoporosis.
In general, endocrine diseases alter the body's delicate metabolic and regulatory balance. When this balance is compromised, bones can become fragile, muscles can weaken or experience cramps, and joints can become inflamed or wear out, resulting in pain and decreased function.
How to maintain hormonal balance and protect your bone health
Maintaining hormonal balance can be challenging, but it's key to your overall well-being and to preserving bone strength.
Get annual medical checkups
Even without obvious symptoms, annual checkups allow us to prevent. Some basic studies your doctor may request include:
- Complete blood count: Evaluates blood cells.
- Blood chemistry: Analyzes elements in blood serum.
- Urine test.
Depending on results, your doctor may refer you to specialists (traumatologist, endocrinologist, gynecologist) or indicate a multidisciplinary approach.
Some hormonal imbalance symptoms include:
- Changes or absence of menstruation.
- Fatigue.
- Skin changes (dryness, darkening on neck or armpits, acne).
- Joint or bone pain due to tissue edema, mainly affecting feet, ankles and legs, which over time can generate more complex orthopedic problems.
Balanced and specialized eating plan
Diet directly influences hormone production and bone health. Try to include:
- Healthy Fats: For hormone production like fish, chia nuts and seeds. Coconut oil and avocado are also excellent omega-3 sources.
- Quality Proteins: Opt for chicken, fish, eggs and legumes essential for tissue repair and growth.
- Fiber and Vegetables: Fiber helps eliminate excess hormones from the body.
- Antioxidants: Protect from oxidative stress that can affect hormonal balance. Berries, citrus, green tea and vegetables are excellent sources.
- Regular Meal Schedule: Avoid skipping meals and try to include protein in each one to maintain stable blood sugar.
- Adequate Hydration: Drink enough water. Limit sugary drinks and caffeine, as they can interfere with your hormones.
Exercise and physical activity
Movement is your best ally against bone loss. Try to combine:
- Brisk walks of at least 30 minutes.
- Strength exercises to maintain muscle and bone mass.
- Low-impact activities like swimming or yoga.
Doing physical activity 3 to 5 days a week will make a big difference.
Stress regulation
Stress, particularly cortisol release, can alter your hormones. To combat it, incorporate deep breathing exercises, have a support network you can talk to, prioritize quality sleep so your body has enough time to recover.
Although at first glance bones and hormones may seem unrelated, they actually work intrinsically together. The body is an orchestra, hormones are the conductors guiding the symphony ensuring balance between bone tissue formation and resorption.
An imbalance, no matter how small, can have significant repercussions, manifesting in conditions like osteoporosis, joint and muscle pain, and even increased susceptibility to fractures. Therefore, understanding the influence of key hormones like estrogen, vitamin D, calcitonin and cortisol is fundamental for prevention and management of these conditions.
Prioritizing regular checkups, adopting a balanced diet, maintaining a consistent exercise routine and managing stress not only contributes to overall hormonal balance, but is also a crucial investment in the strength and health of our musculoskeletal system that allows us to move with integrity and independence.
If you're interested in scheduling a consultation with me, it will be a pleasure to be part of your process. I'm located in Tijuana, Baja California in Torre Norte 2.
You can send me a message from this page and I'll respond promptly, or call me directly to schedule your appointment.
No hay comentarios para este blog.
