Do you have constant pain and inflammation in your arms, legs, or feet?
Have your daily activities recently become difficult to perform due to these discomforts?
If you have had pain and inflammation for more than three months, it's important to see your orthopedic doctor as soon as possible. This could be due to various conditions such as rheumatoid arthritis or very commonly bursitis.
Now, let me explain in detail what this last condition is:
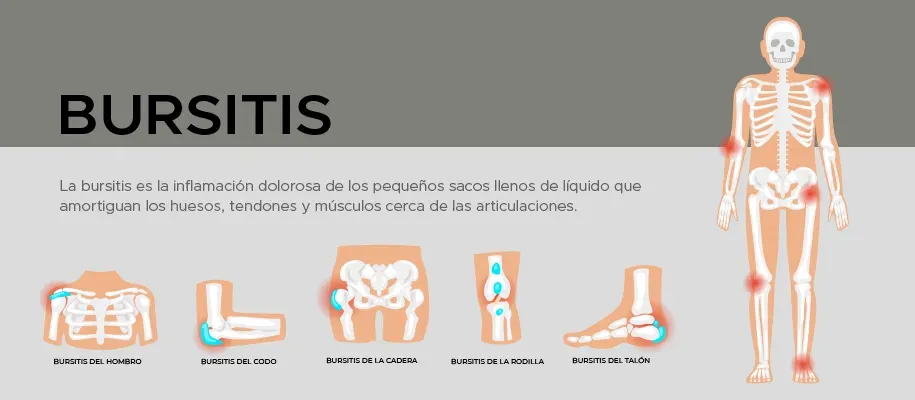
What is bursitis?
To understand it, let's first talk about anatomy. In our body there are several places where a lot of friction is created between tissues, especially around joints and areas where the bone is very close to ligaments or tendons.
To protect itself from this friction, the body has small 'bags' called synovial bursae that are filled with synovial fluid.
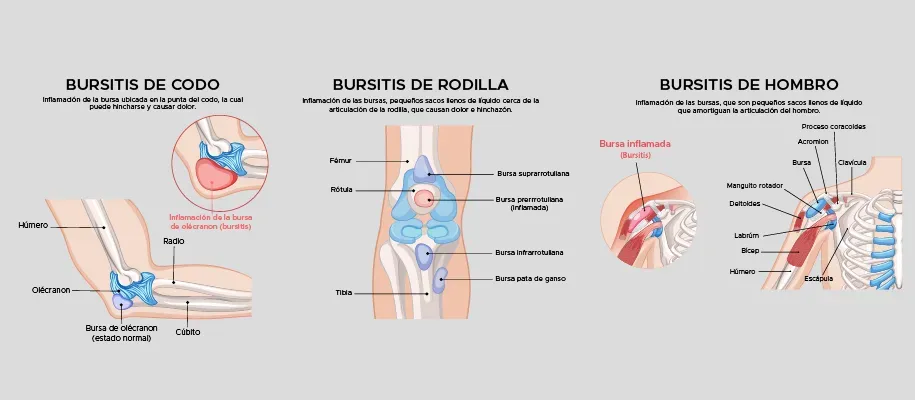
Our body has about 150 bursae. The most notable ones are found around the ankle, hip, knee, shoulder, and elbow. Some are more superficial like in the elbow and others deeper like in the hip.
The problem arises when these bursae become inflamed. When this happens, the synovial cells begin to produce more fluid, which increases pressure and generates pain.
Types of bursitis and their causes
Bursitis is mainly divided into two types: inflammatory and septic (infectious). The most commonly affected areas are the elbow (olecranon) and the knee (prepatellar and infrapatellar).
Inflammatory bursitis: Its causes are usually excess pressure in the area, overuse (repetitive movements), inflammatory arthritis, or a direct blow.
Septic bursitis (infectious): Occurs due to the entry of bacteria through the skin over an already inflamed bursa, or because the bacteria arrives through the bloodstream. This causes a lot of pain and requires immediate attention.
Differences between inflammatory and septic bursitis:
| Signs and Symptoms | Inflammatory | Septic |
|---|---|---|
| Fever | None | Greater than 38°C (in 20% to 58% of cases) |
| Local heat | Present in 50% of cases | Present in 100% of cases |
| Pain | Medium | High and severe |
| Skin conditions | 25-50% of cases | 60-100% of cases |
| Glucose in synovial fluid | Serum glucose greater than 70% | Serum glucose is less than 50% |
What are the general symptoms?
If it's sudden (Acute): it can manifest with pain when the bursa is compressed or stretched during movement. It often limits the range of motion.
If it's chronic (Several months): It usually has frequent recurrences. Flare-ups can last a few days or several weeks. Inflammation near a joint may persist and cause total limitation of the range of motion.
Who does it affect? Risk factors
This condition is common in certain areas due to trauma, infections, and wear from repetitive movements.
Elbow (Olecranon bursitis): It's very frequent here. Athletes, plumbers, carpenters, mechanics, miners, and soldiers have a predisposition to elbow bursitis due to the type of physical work they perform.
Knee (Patellar bursitis): Septic (infectious) bursitis is most frequently located in the knee bursae and is frequently associated with patients suffering from diabetes mellitus.
Among the professions with predisposition to knee bursitis are people who exert constant pressure on that area, such as:
- Masons (especially when working on roofs or floors)
- Gardeners
- Carpet or floor installers who spend hours on their knees
There are several bursae in the knee:
- Prepatellar bursa: The prepatellar bursa is located between the kneecap and the superficial tissues.
- Suprapatellar bursa: The suprapatellar bursa is located between the femur and the quadriceps tendon and communicates with the knee joint. It is often called the suprapatellar recess.
- Infrapatellar bursa: The infrapatellar bursa is actually made up of two bursae located in the distal portion of the patellar tendon, near the tibial tuberosity. They are described as superficial and deep, according to their relative location with respect to the patellar tendon.
How is it diagnosed?
Clinical evaluation and physical examination:
- Visual inspection: Looking for inflammation, muscle atrophy, postures to avoid pain, and skin disorders.
- Palpation: Looking for 'trigger points' of pain and muscle contractures.
- Joint Range: Checking how much the joint can move.
Imaging studies: Ultrasound or Magnetic Resonance (MRI), especially in deep bursitis.
Aspiration (Arthrocentesis): Extract fluid to analyze if there is infection or hemorrhage (due to trauma or anticoagulants).
Treatment:
Treatment depends entirely on what type of bursitis it is.
If it's inflammatory (non-infectious):
The approach is usually conservative:
- Anti-inflammatory physical means (ice)
- Adaptation and change of activities to reduce friction
- The option to extract the fluid and infiltrate the area may even be considered
If it's Septic (Infectious): It's more common in superficial bursae and changes the entire outlook. Depending on the severity:
- Blood glucose management is crucial (if there is diabetes)
Pharmacological therapy: NSAIDs (non-steroidal anti-inflammatory drugs) and oral or topical analgesics are used. Steroids are reserved for when physical therapy and NSAIDs have failed.
In severe aseptic or septic cases, drainage and antibiotics are necessary. If the case is very severe and doesn't respond, surgical intervention may be required to remove the affected bursa.
The physiotherapeutic approach:
Physical therapy is key and includes combined strategies:
- Temporary joint rest
- Cryotherapy: Cold application for 7 to 10 minutes
- Massages to generate analgesia in the region
- Exercises and stretches: To increase circulation, dissolve adhesions, stretch contracted muscles, and relax.
- Passive: Movements without much effort to avoid contractures.
- Active and resisted: To correct muscle disorders and gain resistance and strength.
Prevention: How to avoid bursitis?
Bursitis is a common condition that increases with age or with repetitive activities. The best way to avoid it is to stay active, flexible, and strong, taking conscious measures:
- Place a cushion under your joints when kneeling or putting pressure on your elbows.
- Take active breaks or frequent rests during repetitive tasks.
- Exercise regularly, but start new activities or exercise routines slowly.
- Strengthen the muscles around the joints.
- Stop any physical activity if it causes a lot of discomfort or pain.
- Use both hands to hold heavy tools.
- Wear comfortable, low-heeled shoes.
- Adopt good posture when performing daily activities.
I'm located in Tijuana, Baja California, I'm an orthopedic traumatologist specializing in joint injuries, arthroplasty, arthroscopy, and spine surgery. I also offer online consultations for patients from other states.
Don't hesitate to contact me to schedule an evaluation, learn about your case, and together choose the best treatment plan according to your situation.
You can contact me directly at 664 169 0650 or at my email: pacientes@mongeortopedia.com
No hay comentarios para este blog.
