Proximal Humerus Fracture in Older Adults: Treatments and Recovery Times Explained
Let me briefly explain what the humerus is - it's the longest bone in the arm, connecting the shoulder joint to the elbow. Several muscles intersect here, including the biceps, triceps, and deltoid.
Did you fall on your outstretched arm and fracture your humerus?
Proximal humerus fractures are the third most common fractures, with about 75% occurring in adults over 65 with osteoporotic bone after a fall. A humerus fracture can be painful and significantly limit arm mobility.
Besides age and osteoporosis, other risk factors include vitamin D deficiency, history of previous falls, or prolonged use of certain medications like corticosteroids that can cause degenerative changes in joints, making them stiffer and weaker.
Additionally, joints can undergo degenerative changes that reduce flexibility and increase stiffness, promoting joint problems and making falls more likely.

How does proximal humerus fracture occur?
When falling, it's almost instinctive to extend or 'put out' your arms, which can cause this fracture. Falls don't necessarily need to be dramatic or high-impact to injure and fracture the humerus; with age and bone loss, one becomes more prone.
Age, bone health, nutrition, and complexity of the fall play a determining role in choosing a specific treatment. Often patients present with osteoporosis, significant wear, or diabetes which can place them in a vulnerable situation during the fracture healing process.
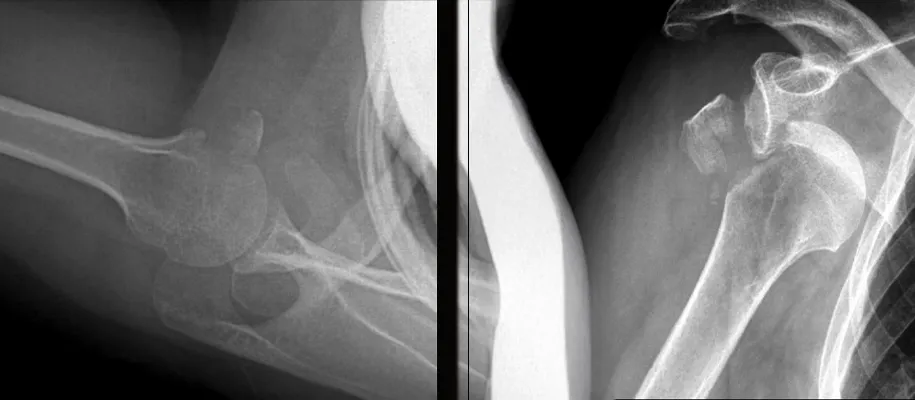
Types of humerus fractures according to Neer classification
The Neer classification divides proximal humerus fractures into four types, according to their complexity:
- Non-displaced fracture: The bone breaks but the parts remain in place.
- Two-part fracture: One fragment of the bone moves, usually in the area of the humeral neck or the tuberosities (protruding parts of the bone).
- Three-part fracture: Two bone fragments are displaced, which can cause shoulder deformity.
- Four-part fracture: The most severe, as all parts of the bone are displaced, increasing the risk of complications such as lack of circulation in the affected area.
Conservative and surgical treatment
Treatment will depend on the type of fracture. For minimally displaced fractures, immobilization is recommended. In more complex fractures, surgery may be necessary, such as osteosynthesis with plates and screws, the use of intramedullary nails, or in more severe cases, a shoulder arthroplasty.
What is daily life like with conservative treatment?
During the first week, pain and discomfort are inevitable. It's essential to maintain relative rest but ensuring movement of the hand, fingers, wrist and elbow to reduce inflammation and prevent stiffness.
Recovery phases
- Pain control
- Learning movements for daily activities (dressing, grooming, sleeping with immobilization).
- Passive movements and periscapular exercises
- Active mobilization of wrist and fingers
- Isometric and isotonic exercises to maintain strength
- Phase II (2-6 weeks):
- If there's no risk of displacement, immobilization use can be reduced and mobility exercises begun.
- Phase III (6-12 weeks):
- Aim to recover maximum active range of motion
- Strengthening shoulder muscles
- Gradual return to daily and sports activities
- Phase IV (3-6 months):
- Maximize strength and joint range with physiotherapy
- Gradual incorporation of sports like swimming. Contact sports like basketball or soccer will depend on the degree of bone consolidation.
- If there's no risk of displacement, immobilization use can be reduced and mobility exercises begun.
- Aim to recover maximum active range of motion
- Strengthening shoulder muscles
- Gradual return to daily and sports activities
- Maximize strength and joint range with physiotherapy
- Gradual incorporation of sports like swimming. Contact sports like basketball or soccer will depend on the degree of bone consolidation.
